Posted on June 11, 2018
After two years of suffering, Pain Rehabilitation Program teaches Nathan ‘you control the pain’
After she broke her ankle in 2016, it was several months before Nathan Parnell was able to put any weight on her injured ankle. Her recovery proved difficult, and Nathan endured disabling pain that reverberated through her legs, hips and back. She struggled for nearly two years before being referred to the Pain Rehabilitation Program at Mary Free Bed.
“I was having problems just walking, squatting, standing …,” said Nathan, a Wyoming, Michigan resident.
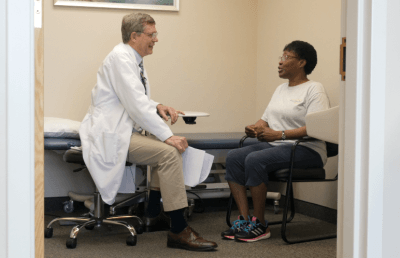
She spent about 10 1/2 weeks under the care of Dr. James Hudson, the program’s medical director, and his team of therapists.
“When you get into the program here, they let you know the pain’s real, you’re not imagining it,” Nathan said. She also learned “that the pain doesn’t have you, you control the pain.”
In this video, Nathan shares how the program taught her to manage her pain and resume a “more normal life.”
“I’m not 100 percent, but I’m doing things I haven’t been able to do in quite some time without so much pain,” she said. “My life is back on track, and that’s awesome. I’m very appreciative of the program and the staff.”